EXCRETORY PRODUCTS AND THEIR ELIMINATION
INTRODUCTION
- Removal of waste products from the body is called excretion.
- Waste products are synthesized in the cells due to metabolic activity.
- Excretion is an essential process in all forms of life. In one celled organisms, waste are discharged through the surface of the cell. The higher plants eliminate gases through the stomata or pores present on the leaf surface. Multicellular animals have special excretory organs.
- Ammonia, urea and uric acid are the major forms of nitrogenous wastes excreted by the animals.
- Ammonia is the most toxic form and requires a large amount of water for its elimination, whereas uric acid, being the least toxic, can be removed with a minimum loss of water.
- On the basis of main excretory products, animals can be divided into 3 groups – ammonotelic, ureotelic and uricotelic (described later).
EXCRETORY ORGANS
- In humans, primary excretory organs are kidney (described later) and accessory excretory organs are lung, liver, skin (sebaceous gland) and intestine.
- Our lungs remove large amounts of CO2 (18 litres/day) and also significant quantities of water every day.
- Liver, the largest gland in our body, secretes bile-containing substances like bilirubin, biliverdin, cholesterol, degraded steroid hormones, vitamins and drugs. Most of these substances ultimately pass out alongwith digestive wastes.
- Sebaceous glands eliminate certain substances like sterols, hydrocarbons and waxes through sebum. This secretion provides a protective oily covering for the skin.
- Intestine – Excess salt of calcium, magnesium and iron are excreted by epithelial cells of colon (large intestine) along with faeces.
- Excretory organs in other animals are – protonephridia, nephridia, malpighian tubules, antennal glands etc.
- Protonephridia or flame cells are the excretory structures in platyhelminthes (flatworms, e.g., Planaria), rotifers, some annelids and the cephalochordate - Amphioxus. Protonephridia are primarily concerned with ionic and fluid volume regulation i.e., osmoregulation.
- Nephridia are the tubular excretory structures of earthworms and other annelids. Nephridia help to remove nitrogenous wastes and maintain a fluid and ionic balance.
- Malpighian tubules are the excretory structures of most of the insects including cockroaches. Malpighian tubules help in the removal of nitrogenous wastes and osmoregulation.
- Antennal glands or green glands perform the excretory function in crustaceans like prawns.
Table : Excretory organs of different organisms (Invertebrates)
EXCRETORY PRODUCTS & THEIR MODE OF EXCRETION
AMINO ACIDS
- These are the end products of protein digestion absorbed into the blood from small intestine.
- Certain invertebrates, like some molluscs (e.g., Unio, Limnae, etc.) and some echinoderms (e.g., Asterias) excrete excess amino acids as such. This is called ammonotelic excretion or aminotelism.
AMMONIA (NH4+ OR NH3)
- It is first metabolic waste of protein metabolism.
- In most animals, excess amino acids are deaminated, i.e. degraded into their keto and ammonia groups. The keto groups are used in catabolism for producing ATP, whereas ammonia is excreted as such or in other forms.
- Ammonia is highly toxic and highly soluble in water. Its excretion as such, therefore, requires a large amount of water. That is why, most of the aquatic arthropods, bony and freshwater fishes, amphibian tadpoles, turtles, etc., excrete ammonia.
- This type of excretion is called ammonotelic excretion or ammonotelism.
UREA CO(NH2)2
- This is less toxic and less soluble in water than ammonia. Hence, it can stay for some time in the body.
- Many land vertebrates (adult amphibians, mammals) and such aquatic animals which cannot afford to lose much water (e.g., elasmobranch fishes, marine bony fish, adult frog, earthworms, nematodes) convert their ammonia into urea for excretion. This type of excretion is called ureotelic excretion or ureotelism.
- Normal blood urea level is 18-38 mg/100 ml of blood.
URIC ACID
- Animals living in dry (arid) conditions, such as land gastropods, most insects, land reptiles (snakes and lizards), birds and kangaroo rat (mammal) etc. have to conserve water in their bodies. These, therefore, synthesize crystals of uric acid from their ammonia for the formation of uric acid. Xanthine oxidase enzyme is necessary.
- Uric acid crystals are non-toxic and almost insoluble in water. Hence, these can be retained in the body for a considerable time before being discharged from the body.
- Uric acid is the main nitrogenous excretory product discharged in solid form (pellete or paste). This excretion is called uricotelic excretion or uricotelism.
HUMAN EXCRETORY SYSTEM
- The tissues and organs associated with the removal of waste products (called excretion) constitute the excretory system. Some of these structures constitute the urinary system which is involved in the synthesis, separation and elimination of mainly nitrogenous waste products and other mineral salts.
- Excretory system consists of a pair of kidneys, one pair of ureters, a urinary bladder and a urethra.
KIDNEY
- Kidneys (mesodermal in origin) are reddish brown, bean shaped excretory and homeostatic organ.
- These are situated on each side of dorsal aorta in the inner wall of the abdominal cavity.
- An average sized kidney measures 10-12 cm in length, 5-7 cm in width, 2-3 cm in thickness with an average weight of 120-170 g.
- It is covered by peritoneum on the ventral side.
- The asymmetry within the abdominal cavity caused by the liver results in the right kidney to be slightly lower than the left one.
- The concavity of the kidney is called hilum through which ureter, blood vessels and nerves enter. Inner to the hilum is a broad funnel shaped space called the renal pelvis with projections called calyces.
- Internally, the kidney is divided into two zones – an outer cortex and an inner medulla.
- Cortex is granular in appearance. Cortex contains malpighian corpuscles, proximal convoluted tubule and distal convoluted tubule.
- Cortex is subdivided into alternating radial tracts known as rays and labyrinthes.
- The medulla is divided into a few conical masses called medullary pyramids. Each pyramid together with the associated overlying cortex forms a renal lobe.
- The cortex extends in between the medullary pyramids as renal columns called Columns of Bertini.
- Renal medulla contains loop of Henle, collecting tubules and duct of Bellini.
- Nephrons are the structural and functional units of kidneys.
- Nephrons eliminate wastes from the body, regulate blood volume and pressure, control levels of electrolytes and metabolites and regulate blood pH.
- There are two types of nephrons according to their position in kidney - cortical and juxtamedullary nephron. (Refer table below).
- Basically each nephron is formed of two parts - the Malpighian corpuscles and the tubule.
Fig. : Section of Kidney
Flow chart : Classification of Nephron
- The renal tubule begins with a double walled cup-like structure called Bowman's capsule, which encloses the glomerulus.
- The renal corpuscle or Malpighian body is named after Marcello Malpighi 1628-1694).
- Glomerulus is a capillary (fenestrated) tuft that receives its blood supply from an afferent arteriole of the renal circulation. The remainder of the blood not filtered into the glomerulus passes into the narrower efferent arteriole.
- The diameter of the afferent arteriole is much more than that of efferent arteriole.
- Bowman's capsule is a blind sac which surrounds the glomerulus.
- The epithelial cells of Bowman's capsule called podocytes are arranged in an intricate manner so as to leave some minute spaces called filtration slits or slit pores.
Fig. : Nephron
- The tubule consists of three parts - proximal convoluted tubule (PCT), a hairpin (U) shaped Henle's loop (which has a descending and an ascending limb) and distal convoluted tubule (DCT).
- The DCTs of many nephrons open into a straight tube called collecting duct, many of which converge and open into the renal pelvis through the medullary pyramids in the calyces.
- The Malpighian corpuscle, PCT and DCT of the nephron are situated in the cortical region of the kidney whereas the loop of Henle dips into the medulla.
Fig. : Malpighian body
- The efferent arteriole emerging from the glomerulus forms a fine capillary network around the renal tubule called the peritubular capillaries. A minute vessel of this network runs parallel to the Henle's loop forming a 'U' shaped vasa recta. Vasa recta is absent or highly reduced in cortical nephrons.
URETERS
- Ureters are narrow tubes started as a pelvis within kidney opening into a common urinary bladder which opens outside through urethra.
- Peristalsis of ureter checks the regurgitation of urine as it undergoes peristalsis to pass urine from kidney to urinary bladder.
URINARY BLADDER
- Urinary bladder is a sac like structure which stores urine temporarily.
- Urinary bladder has two parts-body & trigon.
- Body is made of involuntary muscles which is called detrusor muscle and trigon is a triangular part.
- There are two sphincters on the lower end of trigon –
- Internal sphincter, made of unstriated muscles.
- External sphincter, made of striated muscles.
- Urinary bladder has capacity of 700-800 ml. When it is filled upto 300-400 ml of urine then stretch receptors present on wall of urinary bladder are stimulated and impulse is formed. This impulse is carried to S2-3-4 (spinal segment) through pelvic nerve. Parasympathatic nerve fibers are excited and contraction in detrusor muscle and relaxation in internal sphincter occurs. This causes urine to come out (called micturition).
- Lower part of urinary bladder is jointed with urethra.
URETHRA
- The urinary bladder leads into the urethra. In a female, it is quite short, only about 3 to 5 cm long, and carries only urine. It opens by urethral orifice, or urinary aperture in the vulva infront of the vaginal or genital aperture.
- In a male, the urethra is much longer, about 20 cm and carries urine as well as spermatic fluid. It passes through the prostate gland and the penis. It opens out at the tip of the penis by urogenital aperture. In males, the epithelium of spongy urethra is stratified or pseudostratified columnar epithelia, except near external urethral orifice, which is non-keratinized stratified squamous epithelia.
- The prostatic urethra is lined by transitional epithelia, while membranous urethra is lined by pseudostratified columnar epithelia.
UREA FORMATION
- Urea formation occurs in liver through the Ornithine cycle or Kreb's Henseleit cycle.
- For the synthesis of one molecule of urea, 3 ATP are consumed.
- One molecule of urea is formed by the 2 molecule of ammonia and 1 molecule of CO2. 1 molecule of ammonia come from deamination of fat and other molecule of ammonia comes from aspartic acid.
Fig. : Ornithine cycle
URINE FORMATION
• Urine formation involves three main processes - glomerular filtration (ultrafiltration), selective reabsorption and secretion.
ULTRAFILTRATION
- The first step in urine formation is the filtration of blood, which is carried out by the glomerulus and is called glomerular filtration.
Fig. : Ultra Filtration
- On an average, 1100-1200 ml of blood is filtered by the kidneys per minute which constitute roughly 1/5th of the blood pumped out by each ventricle of the heart in a minute.
- The glomerular capillary blood pressure causes filtration of blood through 3 layers, i.e, the endothelium of glomerular blood vessels, the epithelium of Bowman's capsule and a basement membrane between these two layers. Blood is filtered so finely through these membranes, that almost all the constituents of the plasma except the proteins pass onto the lumen of the Bowman's capsule. Therefore, it is considered as a process of ultra filtration.
- The plasma fluid that filters out from glomerular capillaries into Bowman's capsule of nephrons is called glomerular filtrate. It is a non colloidal part and possesses urea, water, glucose, amino acids, vitamins, fatty acids, uric acid, creatine, creatinine, toxins, salts etc.
R.B.Cs, W.B.Cs, platelets and plasma proteins are the colloidal part of the blood and do not get filtered out from glomerulus. Glomerular filtrate is isotonic to blood plasma.
- Effective filtration pressure (E.F.P.)/Net filtration pressure (N.F.P.) is the glomerular blood hydrostatic pressure minus the colloidal osmotic pressure of blood and capsular hydrostatic pressure.
- Glomerular blood hydrostatic pressure (G.B.H.P.) is the force that a fluid under pressure exerts against the walls of its container.
- Blood colloidal osmotic pressure (B.C.O.P) is the osmotic pressure created in the blood of glomerular capillaries due to plasma proteins albumin, globulin, and fibrinogen. It resists the filtration of fluid from the capillaries.
- Capsular hydrostatic pressure (C.H.P.) is the pressure caused by fluid (filtrate) that reaches into Bowman's capsule and resists filtration.
- The amount of filtrate formed by the kidneys per minute is called the glomerular filtration rate (GFR). There is a sexual difference. In male, the rate is 120-125 ml/min, (i.e. 180 litres/day) and in female, it is 110 ml/min. G.F.R. is affected by volume of circulating blood, neural activity, stretch response to pressure of the wall of the arteriole.
180 litre of filtrate is formed per day, out of it, only 1.5 litre of urine is produced per day which is 0.8% of the total filtrate.
- About 1250 ml (25% of cardiac output or total blood) blood circulates through kidneys each minute and of this blood, about 670 ml is the plasma. The latter is called the renal plasma flow (RPF).
- Filtration fraction (FF) is the ratio of G.F.R. to R.P.F.
FF = 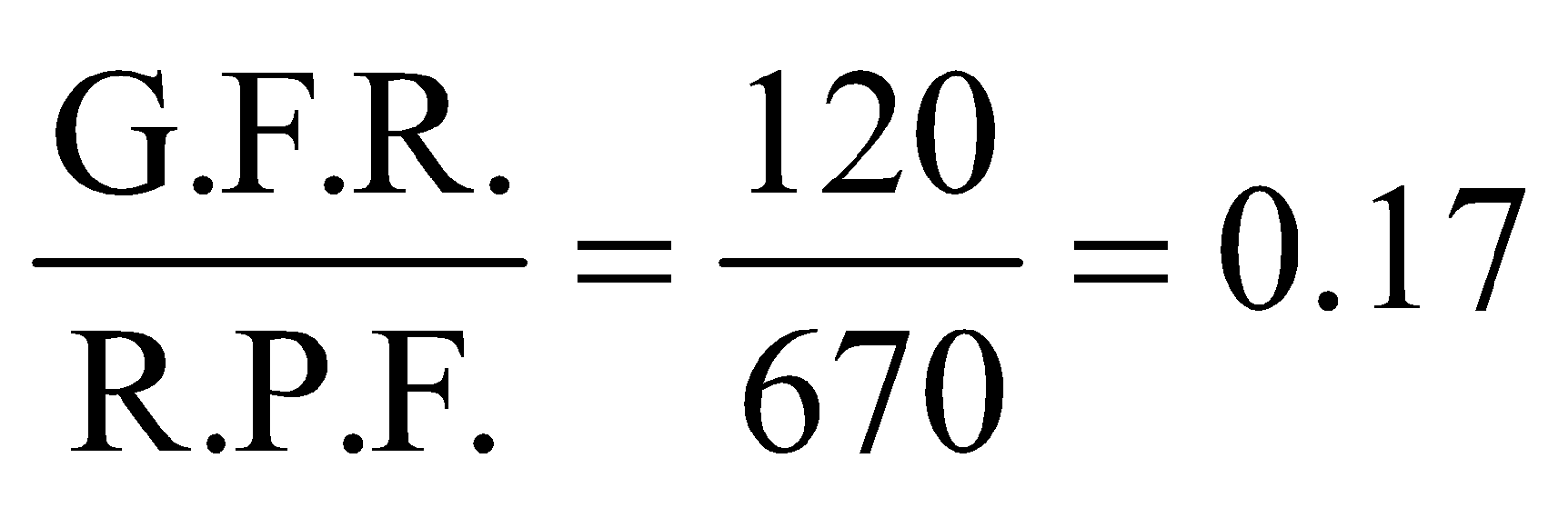
- The kidneys have built-in mechanisms for the regulation of glomerular filtration rate. One such efficient mechanism is carried out by juxta glomerular apparatus (JGA). JGA is a special sensitive region formed by cellular modifications in the distal convoluted tubule and the afferent arteriole at the location of their contact. A fall in GFR can activate the JG cells to release renin which can stimulate the glomerular blood flow and thereby the GFR back to normal.
SELECTIVE REABSORPTION
- Reabsorption is a process due to which the useful constituents of the glomerular filterate are returned into the blood stream.
- The tubular epithelial cells in different segments of nephron perform this either by active or passive mechanisms depending on the type of molecule being reabsorbed.
- During urine formation, the tubular cells secrete substances like H+, K+ and ammonia into the filtrate. Tubular secretion is also an important step in urine formation as it helps in the maintenance of ionic and acid base balance of body fluids.
- Most of the reabsorption takes place within the proximal convoluted tubule.
- Water and urea are reabsorbed by passive transport, by which they move from regions of higher concentration of regions to lower concentration.
- Water is reabsorbed by osmosis and urea by simple diffusion. Water is reabsorbed in all parts of the tubule except the ascending loop of Henle.
- Glucose and amino acids are reabsorbed by active transport.
- The reabsorption of Na+ occurs by both passive and active transport.
SECRETION
- DCT and Collecting tubules constitute the area of tubular secretion.
- It is the active secretion or excretion of waste products from blood capillaries and interstitial fluid into the lumen of nephron.
- It is the opposite of tubular reabsorption.
- Thus, urine is formed in the nephron by a combination of glomerular filteration, tubular reabsorption and tubular secretion.
FUNCTIONS OF THE TUBULES
- Proximal Convoluted Tubule (PCT) involves reabsorption by active transport which is mainly due to large surface area (because of microvilli), numerous mitochondria and closeness of blood capillaries.
- Nearly all of the essential nutrients, and 70-80 percent of electrolytes and water are reabsorbed by this segment.
- PCT also helps to maintain the pH and ionic balance of the body fluids by selective secretion of hydrogen ions, ammonia and potassium ions into the filtrate and by absorption of HCO3– from it.
- Reabsorption in Henle's Loop is minimum, this region plays a significant role in the maintenance of high osmolarity of medullary interstitial fluid. The descending limb of the loop of Henle is permeable to water but almost impermeable to electrolytes. This concentrates the filtrate as it moves down.
Fig. : Reabsorption and secretion of major substances at different parts of the nephron (Arrows indicate direction of movement of materials.)
- Conditional reabsorption of Na+ and water takes place in Distal Convoluted Tubule (DCT). DCT is also capable of reabsorption of HCO3– and selective secretion of hydrogen and potassium ions and NH3 to maintain the pH and sodium-potassium balance in blood.
- Collecting duct extends from the cortex of the kidney to the inner parts of the medulla. Large amounts of water could be reabsorbed from this region to produce a concentrated urine. This segment allows passage of small amounts of urea into the medullary interstitium to keep up the osmolarity. It also plays a role in the maintenance of pH and ionic balance of blood by the selective secretion of H+ and K+ ions.
MECHANISM OF CONCENTRATION OF THE FILTRATE
- A counter current mechanism is the process due to which the urine is made hypertonic.
- Juxtamedullary nephrons are important in counter current mechanism.
- It is the exchange of Na+ ions between the two limbs of the loop of Henle and those of vasa recta (capillary parallel to Henle's loop).
- The filtrate gets concentrated as it moves down the descending limb but is diluted by the ascending limb. Electrolytes and urea are retained in the interstitium by this arrangement.
- DCT and collecting duct concentrate the filtrate about four times, i.e., from 300 mOsmol L–1 to 1200 mOsmol L–1, an excellent mechanism of conservation of water.
VASA RECTAE
- These are blood vessels running parallel to loop of Henle forming a counter current system in juxtamedullary nephrons.
- These are the continuation of efferent arterioles.
- The slow blood flow of vasa rectae is responsible for maintaining the hyperosmolality of interstitium.
Fig. : Counter current mechanism
REGULATION OF KIDNEY FUNCTION
- The hypothalamus, JGA and to a certain extent, the heart regulate the functioning of the kidneys by hormonal feedback mechanisms.
- Osmoreceptors in the body are activated by changes in blood volume, body fluid volume and ionic concentration.
An excessive loss of fluid from the body can activate these receptors which stimulate the hypothalamus to release antidiuretic hormone (ADH) or vasopressin from the neurohypophysis.
ADH increases water reabsorption by the distal tubule and collecting tubule, thereby preventing diuresis. An increase in body fluid volume can switch off the osmoreceptors and suppress the ADH release to complete the feedback.
- ADH can also affect the kidney function by its constrictory effects on blood vessels. This causes an increase in blood pressure. An increase in blood pressure can increase the glomerular blood flow and thereby the GFR.
- Dehydration results in an increase in ADH, while water sufficiency results in low ADH allowing for diluted urine.
- Alcohol inhibits the secretion of ADH and thus, increases water loss.
- Due to deficiency of ADH, a disease called diabetes insipidus is caused in which the output of urine may reach 3-40 litre/day in place of normal 1.2-1.8 litre/day.
- The JGA plays a complex regulatory role in renin-angiotensin mechanisms. A fall in glomerular blood flow/glomerular blood pressure/GFR can activate the JG cells to release renin.
Flow Chart : Renin - Angiotensin Mechanism
- An increase in blood flow to the atria of the heart can cause the release of Atrial Natriuretic Factor (ANF). ANF can cause vasodilation (dilation of blood vessels) and thereby decrease the blood pressure. ANF mechanism, therefore, acts as a check on the renin-angiotensin mechanism.
Table : Summary of events occurring in a nephron
MICTURITION
- Human kidneys can produce urine nearly four times concentrated than the initial filtrate formed.
- The process of release of urine is called micturition and the neural mechanisms causing it is called the micturition reflex.
- An adult human excretes, on an average, 1 to 1.5 litres of urine per day.
- Micturition is involuntary in rabbit and children up to 2 years while it is voluntary in adult human.
- Abdominal muscles and diaphragm help in micturation.
- The urine is a light yellow coloured watery fluid which is slightly acidic (pH-6.0) and has a characteristic odour. The yellow colour of the urine is caused by the pigment urochrome which is a breakdown product of haemoglobin from worn out RBC's.
- On an average, 25-30 gm of urea is excreted out per day.
- The urine on standing gives a pungent smell. It is due to conversion of urea into ammonia by bacteria (hence alkaline).
- Presence of glucose (glycosuria) and ketone bodies (ketonuria) in urine are indicative of diabetes mellitus.
DISORDERS OF THE EXCRETORY SYSTEM
- Malfunctioning of kidneys can lead to accumulation of urea in blood, a condition called uremia. It is highly harmful and may lead to kidney failure.
- Kidney failure or renal failure is the loss of the kidney's ability to excrete wastes, concentrate urine & conserve electrolytes. The first kidney transplantation was done in 1954 in Boston and Paris. The transplantation was done between identical twins to eliminate any problems of an immune reaction.
- Renal calculi are stone or insoluble mass of crystallised salts (oxalates, etc.) formed within the kidney due to dehydration, excess uric acid formation, excess calcium intake etc.
- Glomerulonephritis is the inflammation of glomeruli of kidney.
- Pyelonephritis is an inflammation of renal pelvis, calyces and interstitial tissue. It is due to local bacterial infection. Bacteria reach here via urethra and ureter. Inflammation affects the countercurrent mechanism, and the victim fails to concentrate urine. Symptoms of the disease include pain in the back, and frequent and painful urination.
- Cystitis is the inflammation of urinary bladder. It is caused by bacterial infection. Patient has frequent, painful urination, often with burning sensation.
ARTIFICIAL KIDNEY
- Artificial kidney, called haemodialyser, is a machine that is used to filter the blood of a person whose kidneys are damaged. The process is called haemodialysis. It may be defined as the separation of small molecules (crytalloids) from large molecules (colloids) in a solution by interposing a semipermeable membrane between the solution and water (dialyzing solution). It works on the principle of dialysis, i.e., diffusion of small solute molecules through a semipermeable membrane.
- Haemodialyser is a cellophane tube suspended in a salt-water solution of the same composition as the normal blood plasma, except that no urea is present. Blood of the patient is pumped from one of the arteries into the cellophane tube after cooling it to 0°C and mixing with an anticoagulant (heparin). Pores of the cellophane tube allow urea, uric acid, creatinine, excess salts and excess H+ ions to diffuse from the blood into the surrounding solution. The blood, thus purified, is warmed to body temperature, checked to ensure that it is isotonic to the patient's blood, and mixed with an anti-heparin to restore its normal clotting power. It is then pumped into a vein of the patient. Plasma proteins remain in the blood and the pores of cellophane are too small to permit the passage of their large molecules. The use of artificial kidney involves a good deal of discomfort and a risk of the formation of blood clots. It may cause fever, anaphylaxis, cardiovascular problems and haemorrhage.
Fig. : Flow of blood through an artificial kidney for haemodialysis